⚡ Quick Summary
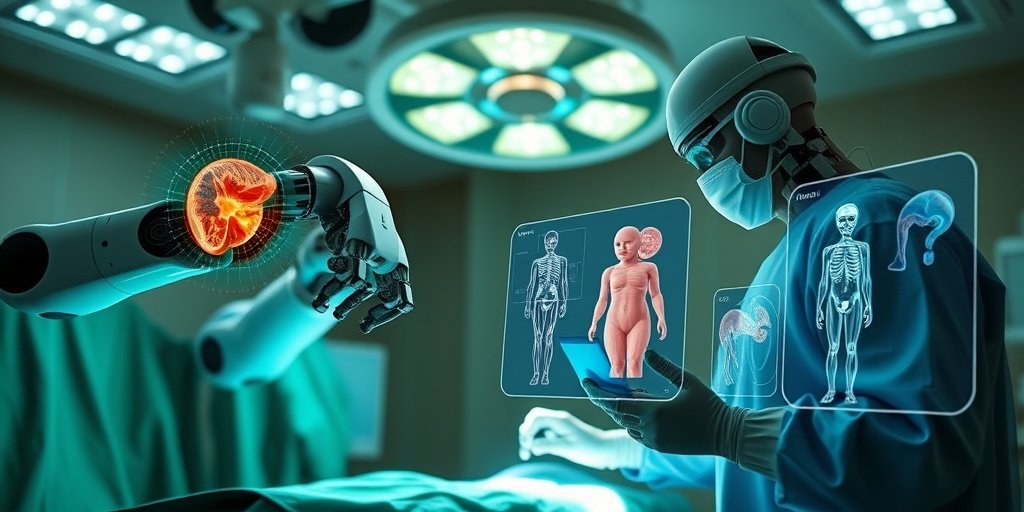
The integration of artificial intelligence (AI) with robotic systems is revolutionizing oncologic surgery, enhancing precision, personalization, and patient outcomes. This review highlights significant advancements and ongoing challenges in AI-driven robotic technologies for tumor resection across various specialties.
🔍 Key Details
- 📊 Scope: AI-powered robotic technologies in oncology, covering urology, neurosurgery, orthopedics, pediatrics, and head and neck oncology.
- 🔬 Evidence: Analysis based on 22 recent clinical studies, pilot trials, and simulation-based research.
- ⚙️ Innovations: Image-free robotic palpation, sensor-assisted feedback, 3D anatomical modeling, and adaptive motion management.
- 🏥 Focus: Tumor boundary detection, real-time intraoperative navigation, and motion compensation.
🔑 Key Takeaways
- 🤖 AI integration is transforming surgical practices, leading to enhanced surgical accuracy and reduced invasiveness.
- 📉 Challenges include inconsistent clinical protocols and limited cost-effectiveness data.
- 🧠 Complex fields like pediatric and neurosurgical oncology face unique anatomical variability and safety concerns.
- 🔗 Interoperable AI-robotic platforms are essential for seamless data integration and real-time analytics.
- 🛡️ Ethical governance and clinician training are crucial for responsible implementation of these technologies.
- 📈 Potential benefits include improved long-term outcomes and reduced recurrence rates through data-driven interventions.
- 🌐 Collaboration among interdisciplinary teams is necessary for successful integration into healthcare systems.
📚 Background
The field of oncology is rapidly evolving, with the integration of AI and robotic systems leading to significant advancements in surgical techniques. These technologies aim to enhance the precision and personalization of surgical interventions, ultimately improving patient outcomes. However, the journey towards widespread adoption is fraught with challenges that need to be addressed.
🗒️ Study
This review critically examines the current landscape of AI-driven robotic surgery in oncology, focusing on various specialties such as urology, neurosurgery, orthopedics, pediatrics, and head and neck oncology. The analysis draws on evidence from 22 recent studies, highlighting both the innovations and the challenges faced in the field.
📈 Results
Key innovations identified include image-free robotic palpation, which enhances tumor boundary detection, and sensor-assisted feedback that improves intraoperative decision-making. These advancements contribute to enhanced surgical accuracy and reduced invasiveness, although challenges such as real-time navigation and motion compensation remain significant hurdles.
🌍 Impact and Implications
The implications of AI-powered robotic surgery are profound, offering the potential to significantly improve patient outcomes in oncology. By enabling minimally invasive interventions and enhancing surgical precision, these technologies could lead to lower recurrence rates and better long-term survival for patients. However, realizing this potential will require addressing existing barriers and fostering collaboration among healthcare professionals.
🔮 Conclusion
AI-driven robotic surgery represents a major shift in the field of oncology, with the promise of improving surgical outcomes through enhanced precision and personalization. As we move forward, it is essential to focus on interdisciplinary collaboration, robust clinical validation, and the establishment of standardized safety frameworks to ensure the responsible implementation of these groundbreaking technologies.
💬 Your comments
What are your thoughts on the integration of AI in robotic surgery? We would love to hear your insights! 💬 Join the conversation in the comments below or connect with us on social media:
AI-driven robotic surgery in oncology: advancing precision, personalization, and patient outcomes.
Abstract
Artificial intelligence (AI) integrated with robotic systems is transforming oncologic surgery by significantly improving precision, safety, and personalization. The review critically explores the current landscape of AI-powered robotic technologies in tumor resection across various specialties, including urology, neurosurgery, orthopedics, pediatrics, and head and neck oncology. Despite rapid advancements, challenges remain in tumor boundary detection, real-time intraoperative navigation, motion compensation, and seamless data integration. Drawing on evidence from 22 recent clinical studies, pilot trials, and simulation-based research, the review identifies key innovations such as image-free robotic palpation, sensor-assisted feedback, 3D anatomical modeling, and adaptive motion management in radiotherapy. These technologies contribute to enhanced surgical accuracy, reduced invasiveness, and improved intraoperative decision-making. However, barriers such as inconsistent clinical protocols, limited cost-effectiveness data, and variability in performance across tumor types continue to hinder widespread adoption. Challenges persist in complex fields such as pediatric and neurosurgical oncology, where anatomical variability and safety concerns demand more advanced solutions. The review emphasizes the need for interoperable AI-robotic platforms, robust real-time analytics, and standardized safety frameworks. It also highlights the importance of ethical governance and clinician training in ensuring responsible implementation. In conclusion, AI-powered robotic surgery represents a major shift in oncology, offering the potential to improve long-term outcomes and reduce recurrence through data-driven, minimally invasive interventions. Realizing the potential will require interdisciplinary collaboration, longitudinal clinical validation, and strategic integration into healthcare systems.
Author: [‘Kok Wah JN’]
Journal: J Robot Surg
Citation: Kok Wah JN. AI-driven robotic surgery in oncology: advancing precision, personalization, and patient outcomes. AI-driven robotic surgery in oncology: advancing precision, personalization, and patient outcomes. 2025; 19:382. doi: 10.1007/s11701-025-02555-3